So if anyone has been following the sepsis debates on the Twitterverse, one of the recurrent issues has been around threshold science. Let’s not forget that sepsis did not define itself. Rather, a bunch of saavy and experienced docs have sat around a table at various times and defined sepsis. Indeed, did not describe it, but defined it.
Now sepsis is a highly heterogeneous syndrome rather than a specific disease, a complex interplay between any number of infectious agents and different host sites and hosts, both sides with different immunological histories.
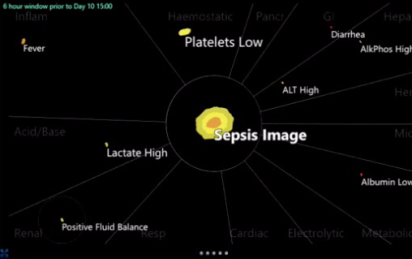
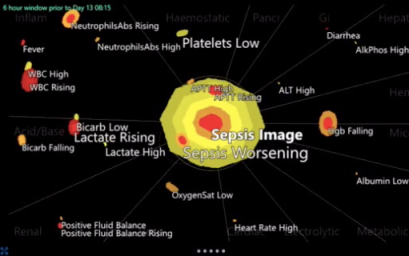
So Lawrence, a veteran ICU doc, has been focusing most of the last decade on developing an extensive clinical data gathering system that delineates relational time patterns of various clinical categories (eg myeloid, hemostatic, respiratory, cardiac). In a sense, this creates a visual matrix that changes over time:
So here is our discussion:
Now what such a tool can be used for I think falls into two categories, the clinical, and more importantly, research, particularly in sepsis.
Clinically, this can be used as a visual tool to monitor and detect failure of therapy (antibiotic resistance) or the development of a second septic source (eg staph pneumonia in influenza). Now one can say that looking at all these data points is what the experienced clinician does, but it isn’t possible to do so, for example, for all my 10 ICU patients in the first second I walk in. On the other hand, a quick look at each patient’s graph, compared to the previous day’s, would immediately flag those who are worsening, and perhaps focus clinical attention and time management in a better fashion. It may even make us catch some we might otherwise have missed, if only by not noticing a platelet drop from 340 to 167 – I could see something like that going under my radar from time to time.
Research-wise, I think this really opens a whole new world, where different phenotypes of sepsis can be potentially described (work we are currently undertaking), and describing the phenotypes (as opposed to arbitrary cutoff definitions) may lead to better categorization and more importantly therapeutic research that may be better tailored to the phenotype.
At some point, AI will be able to learn these patterns, and it will be important that clinicians – much as we double check the machine’s EKG interpretation – understand the patterns themselves.
Lawrence will be at H&R2019 and running workshops on this technology.
Love to hear some comments!
cheers
Philippe