So I posted about this a few weeks ago, and the discussion it brought up with Jon-Emile (www.heart-lung.org) turned out to be way better than the original post, and I just wanted to make sure everyone interested got to see it, so here we go (part 1 is here, for those who didn’t come across it: http://wp.me/p1avUV-bJ):

Jon-Emile: This is a great topic for review Philippe!
I have come across this problem, certainly on more than one occasion. I was first introduced to the idea of renal venous pressure and renal hemodynamics as a house-officer at Bellevue Hospital in New York. Dr. Jerome Lowenstein published work on this phenomenon as it pertained to ‘Minimal Change Syndrome.” He used to ‘wedge’ the renal vein and measure renal interstitial pressure in these patients and measured the response to diuresis. It was very enlightening and made me feel more comfortable given more diuretics in such patients. [Am J Med. 1981 Feb;70(2):227-33. Renal failure in minimal change nephrotic syndrome].
I am also glad that you bring up the cranial vault in this discussion, because I have often wondered if the encapsulated kidneys behave in a similar way. That is, as renal interstitial volume increases from edema, if there is some point on their compliance curve [like the cranium] where there is a very marked increase in renal interstitial pressure? I have found a few articles which loosely address this idea, but would be interested if anyone else knew of some. In such a situation, there would be a ‘vascular waterfall’ effect within the kidneys whereby the interstitial pressure supersedes the renal venous pressure [like West Zone II in the lungs]; then, renal blood flow would be driven by a gradient between MAP and renal interstitial pressure [not renal venous pressure]. I know of one paper that addresses this physiology in dogs, and finds the vascular ‘choke point’ to be in the renal venous system and not Bowman’s space.
What’s even more interesting, is that when renal interstitial pressure is elevated is that the kidney behaves in a sodium avid state [i.e. urine electrolytes will appear ‘pre-renal’] and this physiology has been known for at least a century!
Lancet. 1988 May 7;1(8593):1033-5. Raised venous pressure: a direct cause of renal sodium retention in oedema?
There is no good explanation as to why this occurs, but one I read is that the high renal interstitial pressure tends to collapse the afferent arteriole and the decrease in afferent arteriole trans-mural pressure which facilitates renin secretion [just like low blood pressure would]; but that would require a fairly high renal interstitial pressure unless the MAP was concomitantly low.
Again, what I must caution [and I’ve been personally wrong about this] is the reflex to give diuretics when seeing a ‘plump IVC’. When I was treating a woman with mild collagen-vascular-related pulmonary arterial hypertension, community-acquired pneumonia with a parapneumonic effusion and new acute renal failure, I assessed her IVC with ultrasound. It was plump an unvarying. I lobbied the nephrologist to try diruesis based on the aforementioned reasoning, but was very wrong. Her kidneys took a hit with lasix. What got her kidneys better was rehydration. In the end, what happened was her mild PAH raised her venous pressure and the hypoxemic vaso-constrction from her new pnuemonia only made that worse. Her right heart pressures, venous pressure and probably renal venous pressure were undoubtedly high. But I didn’t take into consideration her whole picture. She had a bad infection, had large insensible losses and had not been eating and drinking. She was hypovolemic, no doubt, despite her high right heart pressures. Fortunately, her pneumonia resolved and fluids brought her kidneys back to baseline.
Thanks again for another thought-provoking topic
Me: Great points as usual Jon, and your last one brings up a bit of a concern I have always had. To play devil’s advocate, one could argue that it may have been resolution of the pneumonia and its metabolic sequelae and possibly other treatment that resulted in improvement of her renal failure, rather than the fluid, no? Did her hypoxia resolution decrease PAP back to normal – with IVC dynamics restoring – and relief of renal congestion, and improvement “despite” fluid?
To me, fluid administration must – at least transiently – increase CO to have any effect on the perfusion side. To do so, my understanding is that it has to go from right to left. Because of the pericardium and interdependence, if RAP exceeds LVEDP, we will start to impair LV preload, which sets up the vicious cycle of a shrinking LV and growing RV. If we can’s increase our RT heart output, obviously our LV CO headed to the kidneys can’t increase either. Hence the assumption would have to be that somehow this additional fluid can – by increasing RV preload (without increasing RV size and further impinging LV?) – help overcome elevated PAP and increase right to left flow. To me, hard to believe without a pericardiectomy (on a short time frame, naturally). Hence I struggle with understanding how a really plump IVC with little variation (if significant pleural pressure variation is occurring) can really still need fluid.
I’d really, really like to get your comments on this. I’ve had a number of conversations about this with people – some of them pretty bright – but none satisfying. Am hoping you can point out my flawed thinking.
Jon-Emile: Philippe, you ask very good questions. Your first point is quite valid. I think we have a bias of assigning meaning to a particular intervention because we think that particular intervention will work. For the patient I treated, we administered multiple drugs [oxygen, antibiotics, bronchodilators, we may have even given a dose of steroids] and yet I assign meaning to the fluids given. I think in all patients with complex hemodynamics that there are multiple co-varying interventions that all [hopefully] push the patient in the right direction – making it quite hard to grant significance to one in particular. Yet in the patient I treated, the timing with respect to creatinine change and urine output made it very hard to argue in favor of diuresis. We were checking her creatinine fairly regularly as she was in step-down and we were concerned about the trajectory of her illness. With lasix, her creatinine jumped abruptly on the following chemistry while with fluids, creatinine dropped and her urine output really picked up.
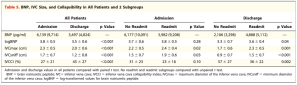
Which brings me to Ulrich’s point. It is well-taken and I hope to have a pulmccm post on this shortly. While the CVP does not have any correlation with volume status or volume responsiveness as you point out, the physiology of the CVP can help explain confusing echocardiographic findings.
All a plump, unvarying IVC with spontaneous inspiration means [if you believe the Guyton, or Magder approach] is that the IVC transmural pressure is remaining on the flat portion of its compliance curve during inspiration.
Click to access cc11824.pdf
In other words, the IVC is at such high volume [on the flat portion] that lowering its transmural pressure [lowering the CVP, raising the intra-abdominal pressure or both] does not cause it to shrink in volume.
The question then becomes why is the IVC in this state? And a great analysis to this question is to consider the determinants of great vein volume [which really is a question of great vein/right atrial pressure or the CVP – which is related to volume by compliance].
There are two primary processes which will raise great vein volume and these flow from the Guyton Diagram 1. excessive venous return 2. poor cardiac function or a combination thereof [its really just inflow versus outflow]. Volume status plays one part of venous return, so certainly, if someone is hugely fluid overloaded, their venous return will be enhanced and this will favour a high great vein volume and high great vein pressure, BUT this will be mediated by cardiac function because if the heart can eject the large venous return it is receiving, then the great vein pressure and volume won’t change or may be low. Conversely, if cardiac function is poor, a patient could have a low venous return [e.g. be hypovolemic or euvolemic] and still have a high great vein volume and pressure – simply, because the heart can’t expel from the thorax what little venous return it receives. Importantly, poor cardiac function can mean almost anything [valve dysfunction, tachycardia with arrhythmia, high afterload, poor contractility, etc.].
To me, the above is the true value of thinking about Guyton and the CVP, so when I approach a patient, I try to think about what their venous return curve looks like [by a clinical exam] and I use a TTE to actually see what their heart function looks like [and to me this is the true power of ICU TTE]. The above also explains why CVP simply cannot be a marker of volume status.
In the patient I was treating, her history and physical really suggested poor venous return [she was clearly with a pneumonia, hadn’t been eating and was euvolemic to dry on examination] yet her great vein volume was high on TTE which meant that her cardiac function was most likely poor [on the Guyton Diagram her low venous return curve would be intersecting a very low, flattened cardiac function curve such that shifts with intra-thoracic pressure would not change right heart pressure at all].
But why was her heart function poor? Why could her right heart not eject what little inflow it was receiving? It was probably a combination of things. The pneumonia probably increased right heart afterload which caused some TR, she was tachycardic so wasn’t getting optimal filling time, she was septic with perhaps some underlying cardiomyopathy, perhaps her diastolic blood pressure was lower than normal [she was an elderly lady with likely stiff arteries] and she wasn’t perfusing her right coronary artery well and was suffering from relative ishcemia] it’s certainly is a lot of hand-waving, but all taken together perhaps plausible.
The antibiotics improved her lung function as did the bronchodilators which lowered pulmonary vascular resistance which improved right heart forward flow, maybe the inhaled beta-agonists increased her contractility, maybe the oxygen also lowered her pulmonary vascular resistance, maybe the steroids sensitized her to catechols and this raised her blood pressure and coronary perfusion pressure which improved her right heart function, but also maybe the fluids? Empirically, and in retrospect, venodilating her with lasix probably really lowered her venous return and this crashed what little cardiac reserve she had. It was improving her venous return with fluids that helped.
Sorry if this post is getting too long …
In terms of ventricular interdependence [an excellent, under-appreciated point in the ICU] I think that you have to be very careful extrapolating whether or not this effect is present from an IVC examination. In a classic paper [that caused much consternation at the time] Pinsky found that right atrial pressure was completely uncoupled from right ventricular end-diastolic volume [why the CVP is a poor indicator of volume responsiveness]. Her is a recent review of that paper by Pinsky himself.
http://www.ncbi.nlm.nih.gov/pubmed/24760121
The take home is that while right atrial volume and pressure [and by corollary great vein volume and pressure] can be high, this may not translate to a right ventricle near its elastic limit. Pinsky offers no good explanation as to why this is, but postulates that it may have to do with the complex RV geometry and how this changes during diastole. So until there is a widely accepted means of assessing RV filling with TTE [like an Ea ratio] which could pick up a restricted filling pattern, this is really hard to call on echo. As you are aware, you could look for a flattened septum or D sign during diastole, but I’m not sure how well that sign predicts a patient’s response to a fluid challenge – it certainly screams caution.
This Pinsky paper also highlights a potential disconnect between the physiology proximal to the tricuspid valve and the physiology below it which is also part of my general reluctance to use IVC volume change as a marker of fluid responsiveness, just as I have total reluctance to use CVP [or its change with respiration] as a marker of fluid responsiveness.
Unfortunately, a lot of the time it comes down to ‘guess and check’ – give fluids or give lasix and see what happens. This is why I firmly believe that determining volume status and volume responsiveness are the hands-down hardest party of ICU medicine.
If you’re still reading, I hope this helps.
One more point. I don’t think I gave a full explanation to one of your questions. Please bear with me as this is exceptionally hard to explain with words [indeed why I made heart-lung.org].
The venous return and cardiac function curves are essentially inverse of each other [that is lowering right atrial pressure increases venous inflow but decreases cardiac outflow] so they approximate the letter X [venous return is the \ and cardiac function is the / & the point at which the two lines intersect make up the CVP and defines cardiac output].
If you consider the patient I described, If we assume her venous return is low [because she is venodilated from sepsis and hypovolemic from low PO] then the venous return curve [\] is shifted leftwards. If we assume her cardiac function is poor the cardiac function curve slope [/] is shifted down and to the right.
When she takes a breath in, the lowering of intrathoracic pressure pulls the cardiac function curve leftwards [lowers its pressure relative to venous return] while the increase in in abdominal pressure with diaphragm decent tends to temporarily increase venous return by decreasing abdominal venous capacitance. This effect shifts the venous return curve in a rightward manner.
If the patient’s venous return curve initially intersects the ascending portion of the cardiac function curve [i.e. she is truly volume responsive] BUT, the intersection is very near the plateau of the cardiac function curve [i.e. the portion of the cardiac function curve that will render the patient non-volume responsive and also favour unvarying respiratory change in right atrial pressure/volume with inspiration], THEN with inspiration it is possible to see the intersection of the two curves on the flat portion of the cardiac function curve [as the cardiac function curve is pulled leftwards and the venous return curve is pushed rightwards], even though she does have some cardiac preload reserve. This would be an example of impaired specificity of IVC volume change with spontaneous inspiratory effort as a predictor of volume unresponsiveness [i.e. a false positive for a plump IVC predicting the lack of fluid responsiveness].
I address this physiology in chapter 6 parts C and D and chapter 8 part F.
Me: Very, very interesting. I think this discussion, as many, show how medicine is not a “hard science” but remains a “pseudo-science”, inherent to the fact that we are blending physics, chemistry, biology and cannot really apply simple principles of flow and pressures when dealing with elastic, muscular systems lined with microscopic coating whose compliance and resistance change from moment to moment and thru effect of neural and hormonal influence. There are simply too many unmeasurable variables to come up with single guidelines and rules.
I think, as you say, that there remains a need for some degree of trial and error, that we are hopefully narrowing with the appropriate application of technology and proper data integration.
I’ll percolate all this and see how I can tweak my mental model!
Thanks a lot Jon-Emile!
Philippe
please visit Jon-Emile at http://www.heart-lung.org

cheers!
…and don’t forget to register for CCUS 2015 at http://www.ccusinstitute.org!!!
Philippe